Flucatuating hormone levels, due to menstruation, ovulation, menopause and/or birth control pill use may play a role in migraine headaches. Where migraines affect slightly more boys than girls before puberty, in adulthood and during adolescence after menstruation begins, about two to three times more women than men suffer from them. Propensity for migraines usually decreases during pregnancy, and post-menopausal women experience fewer migraines than menstruating women, probably the result of lower estrogen, or a balance between estrogen and progesterone levels (instead of the constant hormonal fluctuations seen in women who are cycling) (1). Thus, it would make sense there would be a connection between hormones and migraines.

This lengthy article is going to review how the hormones estrogen, progesterone, testosterone, thyroid, and melatonin influence the propensity for the development of migraines in women. If you like this article and would like even more information, checkout one of my sources for this article from my friend, Suzy Cohen’s great book, Headache Free. If you just want a quick summary, scroll to the bottom to learn my Recommended Plan of Action for Improving Hormonal Balance!
ESTROGEN
Estrogen Drop
As it turns out, a sudden drop in estrogen hormone concentration is a major trigger for migraines in women. Women who are prone to migraines, have migraines predictably around the time of ovulation or menstruation, with the rapid fall in estrogen. Estrogen drops at the beginning of every new cycle in women who are pre-menopausal.
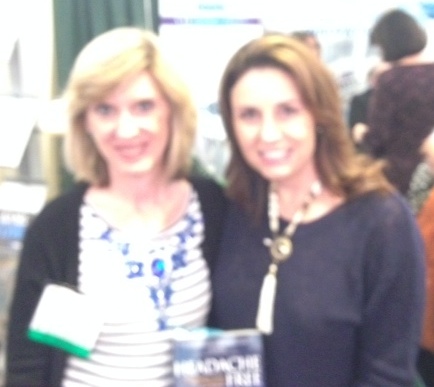
In the normal female hormone cycle, estrogen and progesterone levels are the lowest during the days of menstruation. Day 1 is considered the first day of menstruation or the first day of the follicular phase of the menstrual cycle. Estrogen peaks during the ovulation phase (mid-cycle, around days 10 to 14) of the female hormone cycle. Estrogen and progesterone plummet towards the end of the luteal phase (latter phase of the menstrual cycle), beginning and during the menstruation phase, which is often the trigger for women who are prone to menstrual migraine (2). Steady estrogen levels may improve headaches, thus it’s not about how much estrogen is available on a given day, it’s more about keeping the levels from getting too erratic or chronically elevated.
Estrogen Drop & The Birth Control Pill
The use of the oral contraceptive pill pack can also cause a sudden drop in estrogen, and thus lead to migraines. When the pill is withdrawn for that last week to allow the period to begin, estrogen levels are going to plummet. If you are experiencing migraines with the use of the oral contraceptive pill pack, some women have chosen to use the oral contraceptive, Seasonale, that is taken long term (without a break)—giving you only 4 periods a year, or continuing the administration of the the oral contraceptive without interruption. However, I am not a fan of birth control pills for many reasons, including the fact that they lead to nutrient deficiencies, e.g. vitamin B6, folic acid, zinc, selenium, magnesium and probiotics. It’s very likely that you will be diagnosed with another condition if you are deficient in any of these nutrients and inappropriately be placed on another prescription medication, sadly. (That is the subject of another blog post). There are other options of birth control you might want to consider, that are not subjecting you to a sudden drop in hormone.

Estrogen Drop & The Fall in Serotonin
Estrogen in the brain is in charge of serotonin transport. Serotonin is produced in the intestine and the brain, and is also present in platelets, as well as the central nervous system (CNS). Serotonin has typically been investigated as the feel-good neurotransmitter. When serotonin is low, symptoms of melancholy, anxiety and postpartum depression can ensue. However, serotonin also functions as a hormone, thus allowing serotonin to have physiological consequences in systems outside the CNS.
The falling estrogen of peri-menopause and menopause, can lead to migraines in some females because serotonin effects also drop. When vasodilation occurs in the absence of serotonin’s vasoconstriction effect, the vascular bundles press on nerves to cause neuralgia (face pain) or migraine or headache (3, 4). Serotonin is also a precursor to the hormone melatonin, and thus helps regulate the sleep-wake cycle, and as you will see below, a low melatonin level can also impact the potential for migraines.
However, until estrogen can be better balanced, we can improve serotonin via food and/or supplements and lifestyle adjustments, but be cautious with serotonin-raising supplements if you are taking migraine drugs that are also raising serotonin levels, e.g. triptan headache relievers (like Imitrex), and antidepressants (e.g. Zoloft, Prozac, Celexa, Lexapro, Cymbalta).

Foods to Increase Serotonin:
- Eat foods with plenty of the amino acid, tryptophan, which the body
converts to serotonin. - Foods with high amounts of tryptophan include: avocado, turkey, pork, cottage cheese, wheat germ, wild game.
Supplements to Increase Serotonin:
- Tryptophan, 500-2,000 mg
- 5-HTP, 50-600 mg
- L-theanine, 100-500 mg bid
- Iron, 25-50 mg
- Vitamin B3, 50 mg
- P5P, 50-200 mg
- Vitamin C, 4,000-6,000 mg
- Vitamin D, 1,000-10,000 IU
- MTHF
- calcium
- magnesium
- fish oils
- melatonin
- Passion flower
- vitamin B12
- inositol
- SAMe
- tryptophan
- zinc
- St. Johns Wart, 300 mg tid (caution: has many drug interactions)
Lifestyle Factors to Increase Serotonin:
- boosting aerobic exercise 2-3 times per week for 20-30 minutes
- prayer
- yoga
- meditation
- bright light therapy
- chanting
Estrogen Excess (or Progesterone Deficiency)
Migraines are often also experienced during a time of “estrogen dominance,” or also known as “progesterone deficiency.” Other symptoms experienced with estrogen dominance or progesterone deficiency, other than migraines, include irritability and brain fog, breast tenderness, water retention or bloating, unwanted hair growth, irregular or heavy periods, fibroids and severe PMS and cancer.
The brain is highly responsive to progesterone. Progesterone concentrations are sometimes up to 20 times higher in the brain than in the blood. Progesterone is a calming hormone. If you become deficient it in, your brain responds with severe insomnia, anxiety, and migraine headaches, to name a few of the negative symptoms. Progesterone counteracts the negative effects of estrogen in the brain and the body. Whereas estrogen has an excitatory effect on the brain, progesterone’s effect is soothing. Restless sleep occurs with estrogen dominance, while one will sleep like a baby when balance is restored with bioidentical progesterone. One study has shown that benefit of receiving progesterone during the first few hours after a stroke.
Progesterone works as a natural anti-anxiety drug by improving GABA (gamma aminobutyric acid), an inhibitory neurotransmitter. When trying to eliminate headaches and improve rest, we want more GABA, or we want it to be balanced with glutamate. Progesterone improves GABA and thus helps relieve menstrual migraines. However, until progesterone can be better balanced, we can improve GABA via food and/or supplements and lifestyle adjustments.
Food to increase GABA:
- Foods rich in the amino acid glutamine, which is necessary for the production of GABA: almonds, bananas, spinach, oats, beef liver, halibut, walnuts, tree nuts, lentils, potatoes, broccoli, oranges, rice bran, whole wheat rice
Supplements to increase GABA:
- Glutamine 1,000-3,000 mg
- Magnolia bark (dopamine agonist)
- Inositol, doses up to 2-12 grams
- Vitamin B6 (as P-5-P), 50-200 mg
- Magnesium (succinate) 10 mg
- Thiamine, 400 mg per day
- Niacinamide, 100 mg
- Pyridoxine, 10 mg
- Zinc (glycinate) 5 mg
- Manganese (succinate), 10 mg
- L-Taurine, 150 mg
- Valerian Root extract (standarized to 0.8% valerenic acid) 100 mg
- Passion Flower extract (standarized to 3.5% flavoroids) 100 mg
- L-Theanine, 100-500 mg bid
- Lithium (orotate) 10 mg
Lifestyle Factors to improve GABA:
- aerobic exercise
- work to rid toxic chemicals that accelerate GABA depletion, especially
lead
A progesterone deficiency is also linked with over-activity of pain receptors, as well as abnormally low production of the body’s natural painkillers, called endorphins. A low progesterone also causes reduced production of serotonin, discussed above.
If you are a woman who has had a hysterectomy and are taking estrogen replacement, but not taking progesterone along with it, you are at a very high risk of developing breast cancer and other hormonally-driven disorders, including migraines. At one time, physicians were prescribing estrogen only after hysterectomy, assuming progesterone was no longer needed since there was no longer a uterus. This is poor medicine, since we women have progesterone receptors all over our body, not just in the reproductive organs. Progesterone protects the breasts, and may relieve fibrocystic breast pain and reduce risk of breast cancer, in addition to supporting healthy bones, heart, liver and brain tissue in both men and women.
If any of these symptoms sound like you, I hope you will talk to a healthcare practitioner, such as myself, about prescribing natural progesterone. This is something I can prescribe for you. Natural progesterone is not the same thing as progestin drugs like Provera (medroxyprogesterone) that have been implicated in breast cancer and many other unwanted side effects. I am talking about bioidentical progesterone replacement. Once we evaluate your hormone serum levels, the decision to supplement with progesterone can be evaluated, to help relieve the hormone imbalance.
Estrogen Excess & The Depletion of Magnesium
Elevated estrogen levels lead to magnesium deficiencies. It is well-known that a deficiency in magnesium is a risk factor for migraines. Excessive estrogen, however, can also deplete magnesium levels by influencing adrenal function. The excess estrogen places the adrenals into sympathetic mode (overdrive), leading to severe magnesium wasting (5).

Modulating Healthy Estrogen Levels
I encourage you to see a specialist qualified to assess your serum hormone levels and prescribe (such as myself), if necessary, bioidentical hormones, when needed. However, a healthy diet and natural supplements can help regulate healthy estrogen levels. Unhealthy estrogen metabolites have been shown to be associated with migraines.
First and foremost, make sure your detoxification pathways are open. For more about assuring adequate detoxification, check out my book, Prescription Detox.
One way to assure the effective detoxification of estrogen by-products is to consume sulfur-containing vegetables daily, e.g. broccoli, cabbage, kale, cauliflower, Brussel sprouts and other cruicerfous vegetables.

Natural Supplements for Regulating Healthy Estrogen Levels
- I3C (Indole 3 carbonyl) and/or DIM (Diindolylmethane): DIM is a component of I3C. For people over age 40 years, DIM may actually be a better choice, because in order to convert I3C to DIM, adequate stomach acid (HCl) is needed and many people over 40 years old have reduced stomach acid. (Or contact me to determine if you are a candidate for HCl supplementation). In any case, DIM is completely natural and it encourages the formation of good estrogen metabolites, while decreasing the bad estrogen metabolites that naturally occur with metabolism. In excess, however, DIM may lower thyroid hormone, so be cautious. DIM and I3C are also known to help calm painful menstrual cycles, and support prostate health.
- Vitex Agnus Castus or Chasteberry: this supplement can help support progesterone production. Additionally, it may help with headaches, acne, breast tenderness, depression, premenstrual syndrome, and help normalize irregular cycles by improving ovulation. In menopausal women, it may ease hot flashes.
- Black Cohosh: this herbal remedy and phytoestrogen used in menopause to control hot flashes, and anecdotally, it may help reduce headache frequency. It is also known as mugwort or Cimicifuga reacemosa. Insects hate black cohosh.
- Sage: also known as Salvia Officianalis, sage contains saponins which may ease headaches, especially a headache due to nerves. However, this herb is also estrogenic, so it may not be right for menstruating women, but effective for menopausal women or peri-menopausal women whose estrogen is erratic (and contributing to hot flashes). Sage, a common spice used on poultry, is known as a phytoestrogen like black cohosh.
- Iodine: known as a dietary supplement for thyroid support, iodine has an anti-estrogenic effect, so it could be useful for “estrogen dominance” or progesterone deficiency, a common trigger for migraines. We have three estrogen hormones, and iodine helps balance these three, estrone, estradiol and estriol, by shifting them into a healthy balance (increasing estriol and reducing estrone and estradiol). I do not recommend taking iodine supplements, however, without a practitioner’s guidance, as too much can result in serious consequences. Urine iodine testing is first required (contact me). Preferably rely on healthy diet sources, including kelp, iodized salt and seaweed, and avoid the cumulative effect of the halogens, fluoride, chlorine and bromine, that race for the same spot on the cell that iodine does and prevents the absorption of iodine. We get fluoride from toothpaste and mouthwashes, chlorine from pools and tap water (purchase a chlorine filter and install in kitchen and shower and if a swimmer, iodine supplementation may be needed), and bromine from sports electrolyte drinks, hydrogenated vegetable oil, citrus sodas, flour products and that “new car smell” (that nice aroma is from off-gassing of bromine). Fluoride also attacks the pineal gland which happens to make the hormone melatonin that helps us sleep. Iodine is crucial for thyroid hormone production, as well as for anti-estrogenic effects.
- Calcium D glucarate: supplementing with this supplement may help inhibit beta-glucoronidase activity in the liver (Phase II detoxification), by allowing toxins to get bound up and removed from the body, thereby reducing the risk of hormone-dependent cancers, e.g. breast, prostate, and colon cancer. However, this compound, the calcium salt of D-glucaric acid, is also found in fruits and veggies, especially oranges, apples, grapefruit, and cruciferous vegetables. This supplement is also very beneficial if you have gut dysbiois or digestive issues, because beta-glucoronidase is found in certain bacteria and very pronounced within the gastrointestinal tract due to gram negative bacteria hanging around. With digestive problems comes constipation, making the elimination of estrogen by-products difficult. This supplement is also beneficial for those with an elevated LDL cholesterol or those who predominately eat a meat-based diet, since it lowers LDL levels.
- Chrysin: this herbal supplement acts as a natural “aromatase inhibitor,” similar to the more potent breast cancer drugs, tamoxifen and raloxifene. Aromatization occurs as a result of estrogen being produced by fat cells. Excess aromatase activity occurs in estrogen dominant women, overweight women, and aging men. Additionally, excess aromatase enzyme activity results in testosterone being “aromatized” into estrogen. This can be blocked with an aromatase inhibitor, such as chrysin (or a breast cancer drug). Chrysin calms excessive production of estrogen. It is often compounded right into a bioidentical formula that contains estradiol in it, or it can be taken as a supplement. However, it needs to be used with caution because chrysin is a potent inhibitor of an enzyme MAO-A (monomine oxidase A) and this raises serotonin levels and other neurotransmitters. Some people have a genetic SNP (mutation) in their DNA sequence that is homozygous for MAO-A, which means you already make too much serotonin and other brain chemicals that leave you feeling anxious, panicked, wired, irritable or angry, and therefore, chrysin would not be for you. This is why genetic testing is something everyone should have done. But another reason you might not want to take chrysin is because there are other drugs that you could be taking for migraines that are also raising serotonin levels, e.g. triptan headache relievers (like Imitrex), and antidepressants (e.g. Zoloft, Prozac, Celexa, Lexapro, Cymbalta).
TESTOSTERONE
Low Testosterone
Testosterone replacement is usually associated with males with gonadal disorders resulting in low testosterone. However, the androgen, testosterone has wide ranging biological effects in pre- and post-menopausal women, in part because of widespread androgen receptors found in brain, spinal cord, nerves, breast, bone, muscles, cardio-vascular system, lungs, GI tract, bladder, vaginal tissue, uterus, skin, hair follicles and adipose tissue. Testosterone can also exert its effect indirectly via aromatization to estrogen in these organs, ovary and adrenal gland. Androgen production in women declines gradually throughout the reproductive years. A woman of 40 has approximately half the testosterone of a 21-year old (6).
Recent data has shown that androgens have been effective in the prevention of migraine and other headache disorders. The administration of the steroid medication, Danzol, to premenopausal women was associated with a decrease in the frequency of migraine headache. Another study reported that migraine headaches improved with constant, adequate dosages of estrogen-androgen combinations, as well as testosterone alone in post-menopausal women. Also, a study using pellet implantation gave superior results compared to oral or other parenteral routes of administration, and in a pilot study, continuous testosterone was effective therapy in reducing the severity of migraine headaches in both pre- and post-menopausal women. Still another study reported that testosterone replacement in patients with cluster headaches and low testosterone levels resulted in complete relief of headaches (6).
The mechanism through which testosterone modulates migraine headaches is unknown, but might involve suppression of cortical spreading depression, which is thought to occur during the aura phase of migraine headache. Testosterone is a neuroactive steroid and has been shown to increase serotonin, which may also play a role in prevention of headaches (as previously addressed). The effect of testosterone as a vasodilator, although controversial in the etiology of migraine headaches, may play a role in relief of headaches by stabilizing cerebral blood flow. Furthermore, testosterone has been shown to be both anti-inflammatory and neuroprotective. Thus, there are several possible mechanisms by which continuous testosterone may protect against migraine headaches (6).
THYROID
Low Thyroid
Low thyroid level, termed hypothyroidism can contribute to migraines. With low thyroid hormone production, metabolism (and thinking) slows down, leading to a sluggish or stagnant circulation. This may result in bloating or swelling in the hands and feet that occur right before a headache. Often brain fog sets in and then detoxification pathways become sluggish and toxic waste begins to accumulate. Blood vessels may dilate throughout the body and the blood vessels surrounding the brain may swell, leading to brain fog. Then, a headache may develop. Thus headache may be a symptom of an underachieve thyroid. Thus, if you are taking migraine drugs for your headaches, you are not addressing the true cause of your headache, which is hypothyroidism.
High Thyroid
Headaches are hallmark with high thyroid hormone, probably due to the chronically elevated blood pressure that goes with it. It is possible that if you are on thyroid hormones for hypothyroidism, that the dose is too high. Or, if you are taking medications for hyperthyroidism, to lower the thyroid hormone, it is possible that these medications will also contribute to headaches. In either case, it is crucial to find the proper balance of your thyroid hormone.
Natural Supplements for Improving Thyroid Function
- Iodine: see above “Natural Supplements for Regulating Healthy Estrogen Levels.”
- Selenium: this nutrient is necessary for the conversion of the inactive thyroid (T4) to the active thyroid, T3. Recommended intake of 50-100 mcg daily is suggested and can be obtained by eating two Brazil nuts per day. Other selenium-rich foods include walnuts, tuna, shrimp, eggs, cheese, turkey, beef and oatmeal.
- Ashwagandha: this botanical helps make thyroid hormone and provides antioxidant protection.
- Tyrosine: an amino acid that is needed for production of thyroid hormone and useful to people with hypothyroidism. It should be avoided with hyperthyroidism. Recommended dosage is 50 to 200 mg daily. Nutrients that assist the body in converting the tyrosine to thyroid hormone include B vitamins like B6 and folate, as well as a small amount of copper. Note: avoid tyrosine if you have high blood pressure or cardiac palpitations.
- Mullein: this herb can reduce migraine suffering, while also nourishing the thyroid gland and creating more thyroid hormone.
- Japanese Knotweed: this herb supports thyroid health. It has antioxidant, anti-inflammatory, antifungal and antibacterial properties.
- Zinc: like selenium, this mineral is needed to convert inactive T4 to active T3. Zinc is inactivated by the body by medications, including acid blockers, estrogen-containing hormones and corticosteroids.
MELATONIN
Low Melatonin
There is increasing evidence that headache disorders are connected with melatonin secretion and pineal function. The pineal gland in the brain produces the hormone, melatonin, which acts as the body’s circadian clock. Headaches, often also, have a clearcut seasonal and circadian pattern. Melatonin levels have been found to be decreased in both migraine and cluster headaches. The intensity of pain sensation exhibits marked day and night variations. Since the intensity of pain perception is low during dark hours of the night when melatonin levels are high, melatonin has been implicated as one of the prime anti-nociceptive substances (nociceptive means pain from stimulation of nerve cells). Chronic pain syndromes are often associated with the resynchronization of circadian and biological rhythm, which also cause disturbances in the sleep-wake cycle. Melatonin mechanisms are related to headache pathophysiology in many ways, including (7, 8, 9):
- Antiinflammatory effect
- Toxic free radical scavenging
- Reduction of proinflammatory cytokine upregulation (that leads to pain)
- Nitric oxide synthase activity and dopamine release inhibition
- Membrane stabilization
- GABA and opioid analgesia potentiation
- Glutamate neurotoxicity protection
- Neurovascular regulation
- 5HT modulation
One randomized clinical trial comparing melatonin 3 mg, to amitriptyline 25 mg and placebo, showed that melatonin 3 mg is better than placebo for migraine prevention and more tolerable than amitriptyline and as effective as amitriptyline 25 mg (10). Exogenous melatonin has also been used effectively in the management of pain in medical conditions such as fibromyalgia, irritable bowel syndrome and migraine and cluster headache. Melatonin has been tried during surgical operating conditions and has been shown to enhance both preoperative and post-operative analgesia (11).
Summary:
Eighty percent of people who suffer from chronic headaches, any type, cluster, tension, or migraines, all have a hormonal imbalance, and when you correct that hormonal imbalance, the headaches usually disappear.

Recommended Plan of Action for Improving Hormonal Balance
- See a bioidentical replacement therapy specialist to determine your specific hormone imbalance (estrogen, progesterone, testosterone, thyroid), rather than seeing someone who will give you a prescription for a symptom.
- Assess your micronutrient status, especially if you are on birth control pills that deplete many important nutrients.
- Avoid fake estrogens: remove foods in plastic wrappers or containers that consist of xenoestrogens (fake estrogens), which contribute to the estrogen load. These type of estrogens are more difficult for your body to get rid of, and they disrupt endocrine function. Also, xenoesterogens are found in fragranced popular dryer sheets and laundry detergents, which then permeate your clothing when you wash and dry them, and then come in contact with your skin when you wear them. These can disrupt endocrine function (including the thyroid) (Find out more in my book, Prescription Detox.)
- Assure adequate cholesterol levels (don’t use cholesterol-lowering medications): a healthy cholesterol level is needed to make the hormones estrogen, progesterone, and testosterone.
- Weight loss: excessive fat means excessive estrogen and other hormones that increase headache risk.
- Eliminate artificial sweeteners: they disrupt hormone production.
- Avoid GMO: these foods damage the gut and cause inflammation; avoid GMO soy since it may reduce thyroid activity.
- Eliminate gluten: there is a significant link between wheat gluten allergies and people with thyroid dysfunction.
- Avoid dairy when on thyroid medications: milk and dairy, or mineral-containing supplements containing calcium (and other minerals) will bind with thyroid medication and render it less effective, therefore space them 2 hours apart.
- Eat organic: Pesticides disrupt estrogen and other endocrine hormones. Pesticdes and herbicides sprayed on foods also contains bromine, which suppresses the ability to utilize iodine for thyroid production. If you have the genetic polymorphism, “PON1 gene SNP,” you have more difficulty clearing pesticides from your body well.
- Take the necessary actions to avoid the 3 halogens, fluoride, bromine and chlorine (See above on iodine).
Assure adequate detoxification and methylation pathways: take steps needed to avoid constipation. Assure good gastrointestinal function and take probiotics. Encourage movement, adequate urination and sweating. Assess for the major antioxidant glutathione, that allows for appropriate detoxification and for the maintenance of proper levels of magnesium in the blood. Assure intake of adequate methyl groups and assess for genetic variations that impact these pathways.
- Get good dental care: pathogenic bacteria often cause thyroid and adrenal illness.
- Avoiding melatonin deficiency: main causes are a lack of sleep or anything that disrupts sleep, e.g. shift work, late nights, jet lag, alcohol, caffeine, blood sugar imbalances, stress, exposure to light (particularly blue light), electromagnetic waves and age (some older individuals produce no melatonin at all). Foods that naturally contain melatonin: bananas, morello cherries, sweet corn, ginger, rice, barley, tomatoes, radishes, red wine. Foods that contain tryptophan can also be eaten in the evening as these help induce production of serotonin, which is required to make melatonin: nuts, seafood, turkey and chicken, beans, rice, eggs, whole grains, sesame seeds, sunflower seeds. Micronutrients that are important in melatonin production include: Vitamin B6 (pyridoxal-5phosphate), zinc, magnesium, folic acid. Check out my blog post: “Seven Tips to Improve Brain Health & Overall Well-Being: Make Sleep A Priority.”