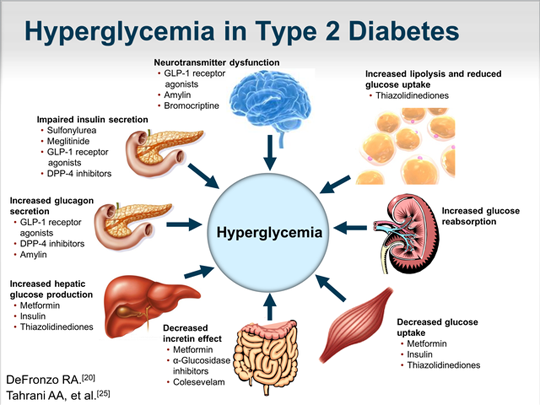
There is an arsenal of diabetes medications that we have today to help us in the fight against type 2 diabetes. Because of the many physiological defects inherent in this condition, one medication class is often not enough.
The “Incretin Mimetic” class of diabetes medications better, known as GLP-1 agonists, are a class of diabetes medications that are not taken orally, but instead are injected similar to the way insulin is injected. However, GLP-1 agonists are NOT insulin.
Why GLP-1 agonists work to improve blood sugar:
There are several system defects in type 2 diabetes. One of these defects found in people with type 2 diabetes is that of decreased effectiveness of the naturally occurring GLP-1 incretin hormone that helps to regulate glucose balance. This hormone is normally produced by the L-cells of the distal ileum (the end part of the small intestine that transitions to the large intestine). This area of the gastrointestinal tract absorbs nutrients and bile after the breakdown of food.
In layman’s terms, “incretin” means “to increase insulin production.“ In the person without type 2 diabetes, GLP-1 is released into the circulation by the intestinal endocrine cells after food is consumed. When GLP-1 reaches the pancreas, it binds to the pancreatic beta cells, thereby enhancing glucose-dependent insulin secretion. “Glucose-dependent” means that this hormone is only released when food is present. In addition to its effects on the pancreas and insulin release, GLP-1 also has the following other antihyperglycemic effects:
GLP-1 agonists stimulates GLP-1 receptors to mimic the effects of native GLP-1, which does the following:
- stimulates insulin release from the pancreatic beta cells in response to high blood glucose levels, and improves first-phase insulin response (in a glucose-dependent manner which protects against hypoglycemia)
- suppresses glucagon release from the pancreatic alpha cells and inhibits glucose production by the liver
- slows gastric emptying and acts on the brain to increase satiety (makes you feel full so you will stop eating).
- Increases beta-cell proliferation and mass and inhibits beta-cell destruction (thereby preserving beta cell activity)
In people with diabetes, response to GLP-1 appears to be slightly blunted, and thus the administration of a GLP-1 agonists is a natural approach to therapy. As a class, the GLP-1 agonists lower A1c by 1% to 1.5%. In addition, GLP-1 agonists may also have beneficial effects on the cardiovascular system, by reducing systolic blood pressure and reducing LDL cholesterol and triglyceride levels.
There are currently FOUR GLP-1 agonists on the market:
1) Exenatide & Exenatide XR:
Short-acting-Exenatide (Byetta®): The patient begins with the subcutaneous injection of 5 ug within 60 minutes before breakfast and supper, and the dose is increased to 10 ug before breakfast and supper after about one month; if not in use, refrigerate until expiration date; if in use: stable at room temperature; discard after 30 days; used when trying to improve post-prandial blood sugars
Long-acting Exenatide (Bydureon®): Initial and max dose are both 2 mg subcutaneously once per week
2) Liraglutide (Victoza®): a long-acting GLP-1 agonist administered subcutaneously that allows for once-daily dosing. Some studies suggest that it may have a slightly greater A1c-lowering effect than exenatide. Liraglutide is typically started at the low dose of 0.6 mg and increased as tolerated to 1.2 mg, and then to 1.8 mg once daily; a non-prandial GLP-1 agonist (provides better FPG control)
3) Albiglutide (Tanzeum®): a long-acting GLP-1 agonist administered subcutaneously that allows for once-weekly dosing. Typically initiated at 30 mg subcutaneously once weekly and increased to 50 mg once weekly in patients requiring additional glycemic control; if a dose is missed, administer within 3 days of missed dose; can be administered any time of the day without regard to meals
4) Dulaglutide (Trulicity®): a long-acting GLP-1 agonist administered subcutaneously that allows for once-weekly dosing; initiated at 0.75 mg subcutaneously once weekly. Dose can be increased to 1.5 mg once weekly for additional glycemic control.
Overall, the GLP-1 agonists are generally well tolerated. They are associated with a low risk of mild or moderate hypoglycemia, and severe hypoglycemia is rare.
Precautions: GLP-1 agonists can cause mild to moderate gastrointestinal adverse events, such as nausea, occasional vomiting, and diarrhea, but these usually subside after 4 to 8 weeks of treatment and can be minimized with dose escalation strategies. Rare but reported side effects have included: jitters, dizziness, headache.
Consider lowering the dose of any sulfonylurea class of diabetes medications the patient may be on, in order to avoid hypoglycemia when starting; GLP-1 agonists may reduce the rate of absorption of other oral medications. Medications requiring threshold concentrations should be taken 1 hour prior to injection.
Contraindications to using GLP-1 agonists: GLP-1 agonists are not for use in patients with type 1 diabetes, severe renal (kidney) disease or end-stage renal disease, or severe gastrointestinal disease, e.g. gastroparesis.
Black box warning: thyroid C-cell tumor warning (avoid if family history of medullary thyroid cancer).
Signs to Alert your healthcare provider of if using GLP-1 agonists: if you get a lump or swelling in your neck, hoarseness, trouble swallowing or shortness of breath, pain in your stomach (often radiating from your abdomen to your back), itching or rash.
Can the GLP-1 agonists be taken with other diabetes medications? Yes. They can be used along with sulfonylureas, metformin, or thiazolidinediones, and insulin in some cases.