So your mother has been diagnosed with Alzheimer’s disease (AD). You have been slowly witnessing the dramatic and devastating changes in her mental demeanor that has transformed her into someone you don’t recognize and who doesn’t recognize you. You have heard that your genes play a big role in determining the possibility of you also becoming a victim of this very debilitating and irreversible neuro-chemical brain disorder, that results in a progressive loss of intellectual function. In fact, statistics show that you are at a 10% to 30% increased risk of developing AD yourself, if you have a first-degree relative with dementia.
More women than men develop AD, and if you are African-American, your risk is even higher. The best-researched genetic marker associated with AD is the APOE-e4 (apoliprotein E gene e4). If an individual is heterozygous (having two copies) for the APOE-e4 gene, they have an 8-fold increased risk of AD.  However, APOE-e is a susceptibility gene, not a determinative gene, which means it increases your risk for getting AD only if modifiable risk factors are not attended to. But also know this about AD: Forty percent of patients with AD do not carry the APOE-e4 gene. This means any of us are potential victims. Therefore, everyone needs to take notice to the potential warning signs and steps that can be taken to avoid becoming a victim of AD.
However, APOE-e is a susceptibility gene, not a determinative gene, which means it increases your risk for getting AD only if modifiable risk factors are not attended to. But also know this about AD: Forty percent of patients with AD do not carry the APOE-e4 gene. This means any of us are potential victims. Therefore, everyone needs to take notice to the potential warning signs and steps that can be taken to avoid becoming a victim of AD.
The Harsh Reality of Alzheimer’s Disease That No One is Talking About:
Alzheimer’s disease is becoming a national epidemic mostly inflicting individuals over 65 years of age, and estimated to affect 5 million of the U.S. population. These days, it is becoming quite common to hear stories such as these: ”missing elderly man found safe,” “elderly woman found dead after wanderin
estimated to affect 5 million of the U.S. population. These days, it is becoming quite common to hear stories such as these: ”missing elderly man found safe,” “elderly woman found dead after wanderin g,” or “search continues for missing elderly woman who wondered off from home.” Unfortunately, it’s mistakenly believed that symptoms, such as getting lost and forgetting who people are, is the beginning of the end of AD. However, these are actually late signs. This dreaded disease actually begins 10-20 years before the symptoms of getting lost or forgetting who people are, and instead the onset of AD manifests with symptoms that are usually ignored and not considered significant.
g,” or “search continues for missing elderly woman who wondered off from home.” Unfortunately, it’s mistakenly believed that symptoms, such as getting lost and forgetting who people are, is the beginning of the end of AD. However, these are actually late signs. This dreaded disease actually begins 10-20 years before the symptoms of getting lost or forgetting who people are, and instead the onset of AD manifests with symptoms that are usually ignored and not considered significant.
We often joke around when people in their middle ages forget something that they previously had no  problems remembering, and kiddingly respond by saying they are experiencing a “senior moment.” But wha
problems remembering, and kiddingly respond by saying they are experiencing a “senior moment.” But wha t if what they are experiencing is the first sign of AD? Do we just wait around to see if they get lost or forget their children’s names? Or do we intervene and start investigating possible risk factors that could be eliminated and potentially prevent this disease from taking foot? I vote for the latter, even though not all of these people showing early signs of AD will develop the disease, there is absolutely no harm in instituting lifestyle interventions that will lead to the most optimum outcomes for overall health and vitality, including the avoidance of AD.
t if what they are experiencing is the first sign of AD? Do we just wait around to see if they get lost or forget their children’s names? Or do we intervene and start investigating possible risk factors that could be eliminated and potentially prevent this disease from taking foot? I vote for the latter, even though not all of these people showing early signs of AD will develop the disease, there is absolutely no harm in instituting lifestyle interventions that will lead to the most optimum outcomes for overall health and vitality, including the avoidance of AD.
What are the Potential Warning Signs of Alzheimer’s Disease?
One of the very first early symptoms of AD is olfactory dysfunction, present in up to 90% of AD patients,  resulting in smell impairment. This does not mean that everyone who has an inability to smell will get AD however, but research now confirms that loss of smell is involved in the early stages, partially due to an imbalance in the olfactory bulb functionality, which is located in the brain’s temporal lobe. The temporal lobe is also involved in short to
resulting in smell impairment. This does not mean that everyone who has an inability to smell will get AD however, but research now confirms that loss of smell is involved in the early stages, partially due to an imbalance in the olfactory bulb functionality, which is located in the brain’s temporal lobe. The temporal lobe is also involved in short to 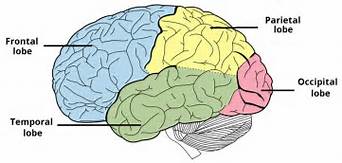 long-term memory conversion and learning and recall (including associating names with faces, inability to recognize places, addresses, routes and location of items). The temporal lobe is also involved with our adrenal circadian rhythm, thus disruption to this system, e.g. disordered sleep patterns, might also be an early sign worth investigating.
long-term memory conversion and learning and recall (including associating names with faces, inability to recognize places, addresses, routes and location of items). The temporal lobe is also involved with our adrenal circadian rhythm, thus disruption to this system, e.g. disordered sleep patterns, might also be an early sign worth investigating.
Other early signs of AD are depression and apathy (lack of feeling, emotion, interest and concern), and/or  being disorganized and distracted (our executive function). The area of the brain involved that is responsible for these tasks is the frontal lobe. The frontal lobe is also involved in our working memory, and eventually, the hallmark sign of AD, is decline in memory. Our learning and memory pathways are a coordinated effort between the frontal lobe and the temporal
being disorganized and distracted (our executive function). The area of the brain involved that is responsible for these tasks is the frontal lobe. The frontal lobe is also involved in our working memory, and eventually, the hallmark sign of AD, is decline in memory. Our learning and memory pathways are a coordinated effort between the frontal lobe and the temporal  lobe. These parts of the brain are also known as the seat of humanity and what divides us from the animal kingdom. It’s where we understand social norms and compassion and love and also where we define our personality. If this part of the brain degenerates, as a result of AD for example, than our personality will begin to disintegrate.
lobe. These parts of the brain are also known as the seat of humanity and what divides us from the animal kingdom. It’s where we understand social norms and compassion and love and also where we define our personality. If this part of the brain degenerates, as a result of AD for example, than our personality will begin to disintegrate.
So What Causes This Brain Degeneration of Alzheimer’s Disease?
AD is a disease that is the result of protein aggregation. As a result of normal metabolism and the use of our brains, proteins are created and used, but then are degraded and cleared out, as long as the body is  functioning as it should. Many processes and mechanisms are required for this degradation and clearing of these proteins, including appropriate nutrients, hormones, enzymes, oxygen, appropriate blood sugar control, and many other factors. But what happens in AD is that our ability to run the clearing process gets compromised, and instead of these proteins being cleared up, they instead clump up together and create aggregates called “Tau Proteins” and “Beta Amyloid Plaques,” which clump together to cause “Neurofibrillary Tangles.” These neurofibrillary tangles and plaquing start to interfere with the synaptic signaling of our neurons. If these brain nerve cells stop firing as a result of the build-up of protein aggregation, neurofibrillary tangles and plaquing, they die and thus the function associated with that part of the brain is lost. As time goes by, these abnormal structures spread from the temporal lobe to the frontal lobe, and from there it progresses to effect the entire brain. The progression varies, depending on the diet and lifestyle of the individual.
functioning as it should. Many processes and mechanisms are required for this degradation and clearing of these proteins, including appropriate nutrients, hormones, enzymes, oxygen, appropriate blood sugar control, and many other factors. But what happens in AD is that our ability to run the clearing process gets compromised, and instead of these proteins being cleared up, they instead clump up together and create aggregates called “Tau Proteins” and “Beta Amyloid Plaques,” which clump together to cause “Neurofibrillary Tangles.” These neurofibrillary tangles and plaquing start to interfere with the synaptic signaling of our neurons. If these brain nerve cells stop firing as a result of the build-up of protein aggregation, neurofibrillary tangles and plaquing, they die and thus the function associated with that part of the brain is lost. As time goes by, these abnormal structures spread from the temporal lobe to the frontal lobe, and from there it progresses to effect the entire brain. The progression varies, depending on the diet and lifestyle of the individual.
Are You Ready to Take the Steps You Need to Prevent Becoming a Victim of Alzheimer’s Disease?
 I hope you said yes to this question. Surely, you don’t want to take chances with the possibility of this disease robbing you and your family of years of a quality life together, knowing there is something you can do to prevent it or slow the progression. Even if the onset of AD could be delayed by even 5 years, the total number of people suffering could be cut in half. The brain cannot regenerate neurons, and therefore, prevention and slowing the progression are the only feasible goals.
I hope you said yes to this question. Surely, you don’t want to take chances with the possibility of this disease robbing you and your family of years of a quality life together, knowing there is something you can do to prevent it or slow the progression. Even if the onset of AD could be delayed by even 5 years, the total number of people suffering could be cut in half. The brain cannot regenerate neurons, and therefore, prevention and slowing the progression are the only feasible goals.
Here’s Where You Can Start:
1) Find out if you have the APOE-e4 gene. Click HERE to purchase this screening test now. If you are found to  have this gene, this gene is modifiable. Research has shown that both exercise and diet decrease the risk of developing AD. However, other research suggests that carriers of this gene are especially vulnerable to heavy metal toxicity, and thus known carriers can take extra precautions to avoid unnecessary metal exposure.
have this gene, this gene is modifiable. Research has shown that both exercise and diet decrease the risk of developing AD. However, other research suggests that carriers of this gene are especially vulnerable to heavy metal toxicity, and thus known carriers can take extra precautions to avoid unnecessary metal exposure.
2) Set up a consultation with me, so we can rule out any adrenal (including sleep and stress issues), micronutrient, thyroid, blood sugar, hormone, anemia or inflammatory conditions, and/or institute the proper diet and lifestyle protocols to decrease the risk and/or progression of AD. Elevated levels of estradiol (estrogen) have been shown to increase the risk of dementia and AD in elderly women, and stress and sleep deprivation contribute to cognitive decline. Inability to properly detoxify can also lead to AD.
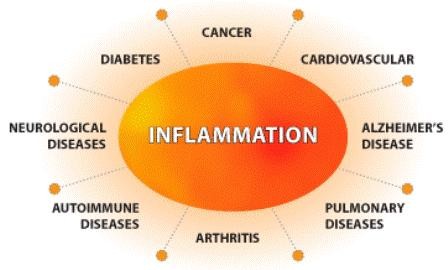 3) If you have symptoms of depression and/or apathy, let’s investigate your nutritional status, and markers of inflammation, since depression is a mainly an inflammatory problem, not a brain disorder. You are not crazy! Sign up for your free gift now that includes more information on how to reduce inflammation.
3) If you have symptoms of depression and/or apathy, let’s investigate your nutritional status, and markers of inflammation, since depression is a mainly an inflammatory problem, not a brain disorder. You are not crazy! Sign up for your free gift now that includes more information on how to reduce inflammation.
4) Engage in mental activity, learning, and social interaction, which has been shown to reduce cognitive deficits by activating brain plasticity and  enhancing the generation of new nerve synapses. Exercising one’s brain is referred to as “building cognitive reserve.” Cognitive exercises early in life seem to provide this reserve: years of education, mentally stimulating pastimes, and intellectually challenging occupations have all been shown to significantly prevent or delay dementia.
enhancing the generation of new nerve synapses. Exercising one’s brain is referred to as “building cognitive reserve.” Cognitive exercises early in life seem to provide this reserve: years of education, mentally stimulating pastimes, and intellectually challenging occupations have all been shown to significantly prevent or delay dementia.
5) If you smoke or are around second-hand smoke or drink alcohol  excessively, work to eliminate these as soon as possible, as they rob your body of oxygen, add to the toxic load, and reduce the ability of your body to detoxify.
excessively, work to eliminate these as soon as possible, as they rob your body of oxygen, add to the toxic load, and reduce the ability of your body to detoxify.

6) If you have diabetes, prediabetes, metabolic syndrome/insulin resistance, or cardiovascular risk factors e.g. high blood pressure and elevated cholesterol, please consult with me so we can work to reverse these conditions. There is a strong relationship between insulin and beta-amyloid metabolism, but contrary to what conventional medicine will have you believe, these conditions are reversible without medications.
7) A diet rich in antioxidants, omega-3 fatty aids and other required nutrients is foun dational for preventing AD. Calorie restriction and intermittent fasting has been shown to protect neurons against plaque formation, and promoting nutritional ketosis is also proving to be transformational. (Using Bulletproof coffee might be a place to start incorporating this “brain octane” fuel that can help induce ketosis). Adherence to the Mediterranean diet is one of the best predictors for longer-term survival.
dational for preventing AD. Calorie restriction and intermittent fasting has been shown to protect neurons against plaque formation, and promoting nutritional ketosis is also proving to be transformational. (Using Bulletproof coffee might be a place to start incorporating this “brain octane” fuel that can help induce ketosis). Adherence to the Mediterranean diet is one of the best predictors for longer-term survival.
 8) There are many supplements (nutrients and herbs) that are showing promise in delaying AD progression, including: acetyl-L carnitine, phosphatidylcholie, phosphatidylserine, B vitamins, vitamin E, ginkgo biloba, Huperzine A, lemon balm, and sage. Please contact me so we can can get you started on the most ideal supplement program for you.
8) There are many supplements (nutrients and herbs) that are showing promise in delaying AD progression, including: acetyl-L carnitine, phosphatidylcholie, phosphatidylserine, B vitamins, vitamin E, ginkgo biloba, Huperzine A, lemon balm, and sage. Please contact me so we can can get you started on the most ideal supplement program for you.
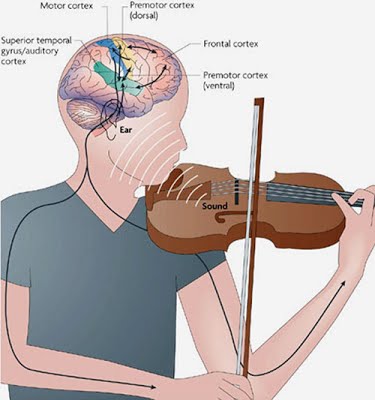
9) Other treatments that have been shown to directly or indirectly help reduce AD: humor, music and reiki.
AD is a devastating disease that significantly affects quality of life and robs years of health and vitality, not just of the victim, but also for the victim’s loved ones. Therapeutic management is complicated. While the initiation of the disease process may have been the result of a simple nutritional deficiency or toxicant, simply correcting the deficiency or removing the toxin may not be enough. Since new neurons cannot be generated the only treatment is improving the health and function of remaining neurons, thus intervention must focus on prevention of slowing the progression of this disease.