Brain fog. Loss of focus and concentration. Poor attention span. Depression. Mood swings. Nervousness. Stress. Anxiety. Wired and tired.
Can you or someone you love relate to experiencing any of these symptoms?
Could your body actually be experiencing an anti-depressant or anti-psychotic medication deficiency?
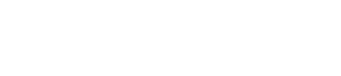
Is it time for Prozac, Zoloft, Celexa, Lexapro, Ritalin, Haldol, Valium, Xanax?

Of course, I am being facetious here, but unfortunately, in today’s pharmaceutical-driven healthcare society, too many healthcare practitioners are pulling out their prescription pads and prescribing anti-depressant or anti-anxiety drugs, such as these, for every neurological-based symptom their patients are experiencing. More often than not, these practitioners are prescribing these drugs before even doing any testing or digging deep enough to determine a cause for their patients symptoms.
Symptoms such as these described above, that appear to be brain-based, can be the result of biochemical imbalances in the body or from biochemical imbalances that have been left untreated for so long that they begin damaging the most basic and fundamental cells of our nervous system—-our neurons.
 Adding an anti-depressant or anti-anxiety medication to this scenario is not solving the problem, but is in fact,
Adding an anti-depressant or anti-anxiety medication to this scenario is not solving the problem, but is in fact,
covering the problem up and only allowing it to fester to the point of further neurodegeneration (loss of structure and function of nerve cells).
Sadly, according to the largest vendor of U.S. physician prescribing data, 78 million Americans are taking psychiatric medications, with over 41 million people being on anti-depressants. About one in 10 Americans, aged 12 and over takes an anti-depressant, according to the Centers for Disease Control and Prevention. Meanwhile, the real cause for people’s neurological symptoms are never addressed, and these bad brains are only getting worse, thus contributing to more serious brain conditions, including Alzheimers, Parkinson’s, Huntington’s diseases and Amyotrophic Lateral Sclerosis, to name a few.
A one size fits all approach to caring for people with these neurological symptoms just doesn’t work. The “one pill, one ill” mentality has got to stop. We are all different with different biochemical needs, and different lifestyles that may be contributing to our real deficiencies, e.g. micronutrient or antioxidant deficiencies, or to our excess of calories and sugar that are having huge impacts on the function of our neurons. Our environmental exposures, that include anything from air pollution to the toxins in our food supply and personal care products can even impact our precious neurons through inflammatory insult. Neurons can also have been damaged as a result of concussions, or mild traumatic brain injury that were incompletely resolved from playing high school sports, for example, and made worse as a result of these other biochemical imbalances. Other individual biochemical factors that could impact neuronal function are, of course, our hormones, but also our genetic variations that can influence our susceptibility to environmental factors and our risk to developing certain health conditions.
 Thus, unless a healthcare practitioner does a thorough assessment and investigation of the person in front of them, in my opinion, prescribing one of these anti-psychotic or anti-depressant drugs is a form of medical negligence. Instead, the healthcare practitioner’s job is to find and fix the mechanisms that are promoting faulty neurological function.
Thus, unless a healthcare practitioner does a thorough assessment and investigation of the person in front of them, in my opinion, prescribing one of these anti-psychotic or anti-depressant drugs is a form of medical negligence. Instead, the healthcare practitioner’s job is to find and fix the mechanisms that are promoting faulty neurological function.
The most fundamental metabolic need for our neurons is to receive adequate blood flow, adequate oxygen and adequate glucose and not be negatively compromised by our environment, stressors and less than ideal lifestyles that can harm our neurons through inflammatory and oxidative insults. Obviously, this is the most basic need for all of our cells, but especially our brain since, being even larger than our heart and kidneys, requires approximately 20-23% of our body’s total energy requirements.

This energy (fuel), in the form of ATP (adenosine triphosphate), is made in the mitochondria (powerhouses of the cells), as long as we provide it with the proper precursors (oxygen, nutrients, glucose, and avoidance of the products of inflammation). As mentioned above, however, the blood flow needs to be adequate to transport oxygen and these necessary precursors, but all too often transport is compromised when a person is anemic. This is why it is crucial to investigate through laboratory analysis if a person has an anemia, e.g. microcytic/hypochromic anemia (iron deficiency), macrocytic/megablastic anemia (vitamin B12 deficiency) or an anemia of inflammation/chro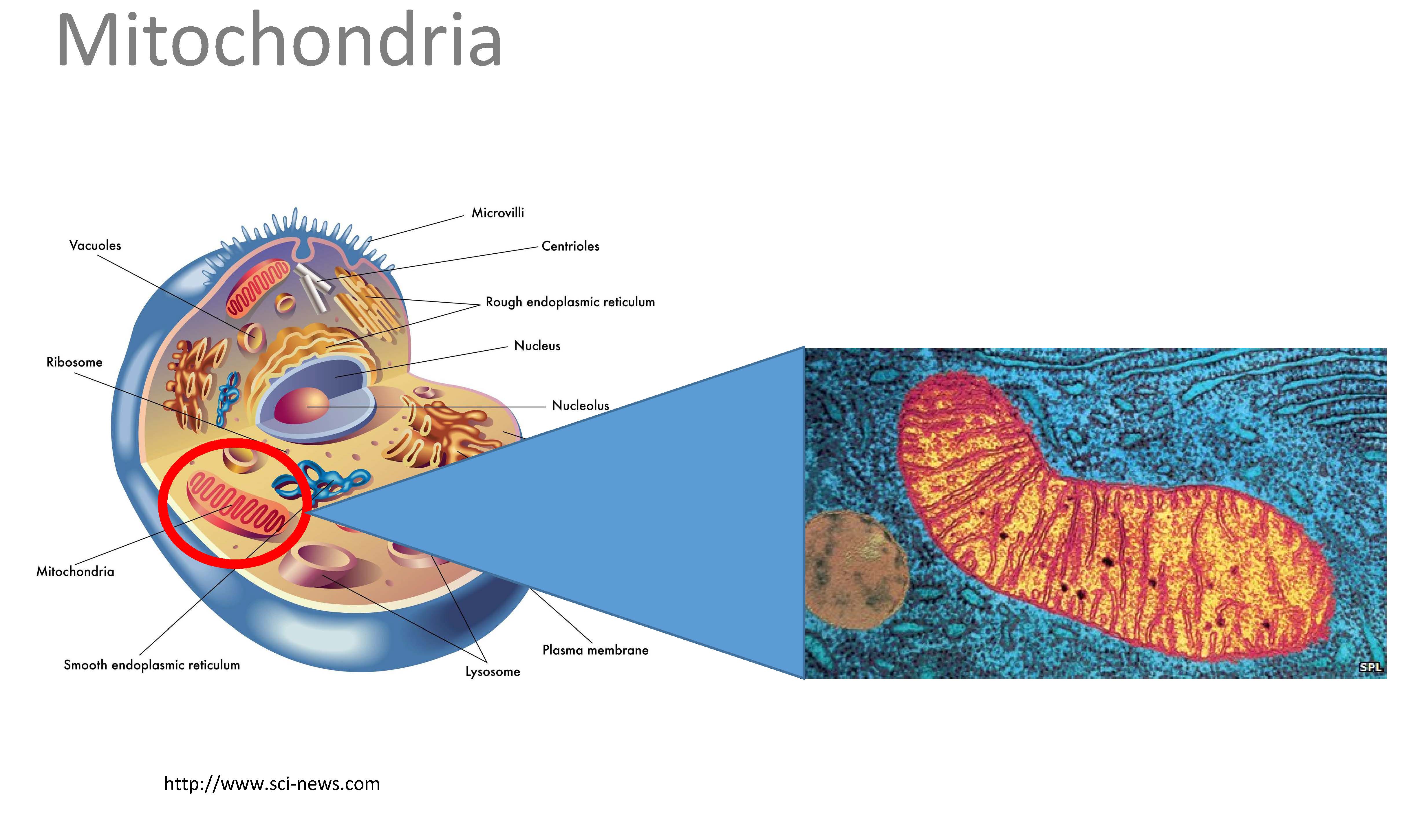 nic disease.
nic disease.
Of course, other things can also compromise blood flow to our brain, including stress, smoking, lack of exercise, poor nutrition, high blood pressure, and conditions e.g. diabetes, which brings me to the next huge problem in our country today that is leading to neurodegeneration, and that is insulin resistance and dysglycemias. Dysglycemia is a broad term that refers to any abnormality in blood glucose levels that lead to disease. Hypoglycemia means low blood sugar, and hyperglycemia means high blood sugar. Hypoglycemia is not a disease, but a symptom and it can result from an overdose of medications used to treat diabetes and/or it can result from an improper diet and eating behaviors. Our brain must have sugar and if it doesn’t receive it, it can compensate through other mechanisms to produce the energy it needs for a short time, but you don’t want to overwhelm the brain by relying on this back-up plan. Eventually it will become too overwhelmed and neurons will die.
On the opposite extreme, there may be an abundance of glucose available, but due to insulin resistance (caused by obesity), a faulty insulin mechanism prevents the neurons from receiving the glucose and consequently, less ATP can be generated and neurons die. The excess glucose that the brain is exposed to can also promote inflammation (similar to toxins, injury, infection, stress, etc.) by leading to the accumulation of advanced glycated end-products (AGEs) (think of your cells as being carmelized and coated with maple syrup). This further causes neurodegeneration. In fact, brain-based insulin resistance is now known to contribtute to the development of Alzheimer’s disease, now known as type 3 diabetes.
Can you see now why the use of anti-psychotic and anti-depression drugs are not the answer to brain- based/neurological symptoms? The answer lies in avoiding anemias, dyglycemias and inflammation to the neurons. In fact, these are absolute deal breakers since ATP cannot be generated otherwise. Therefore a good healthcare practitioner will look for these three things and fix them before prescribing anti-psychotic or anti-depression drugs. Once these three things are optimized, use of these drugs should be a mute point. Our brains are NOT deficient in these medications. Let’s work together to determine what they really may be deficient in.
based/neurological symptoms? The answer lies in avoiding anemias, dyglycemias and inflammation to the neurons. In fact, these are absolute deal breakers since ATP cannot be generated otherwise. Therefore a good healthcare practitioner will look for these three things and fix them before prescribing anti-psychotic or anti-depression drugs. Once these three things are optimized, use of these drugs should be a mute point. Our brains are NOT deficient in these medications. Let’s work together to determine what they really may be deficient in.
The good news is if caught soon enough, mild cognitive impairment and even the early phase of Alzheimer’s disease may be reversed.
I would be honored if you would allow me help you regain neurological function and prevent further neurodegeneration. Get started HERE.